Around the globe, countries looking to improve value for money are investing in systems to build the information base for healthcare decision-making. Where governments are reimbursing healthcare providers, understanding the cost-of-service provisioning is a critical part of this evidence base. Many countries, like the UK and Australia, that have advanced along the universal health coverage (UHC) route have developed sets of healthcare reference costs and costing repositories providing a source of locally appropriate cost data for price negotiations, priority setting, and budgeting. Other countries have relied on sporadic costing exercises or international sources of cost data such as the World Health Organisation (WHO) Choice database. India is no exception. A breakthrough effort in UHC strategy by the Indian government has been the launch of Ayushman Bharat, the government’s flagship scheme, comprising two inter-related components: Health and Wellness Centres and the world’s largest health insurance scheme, Pradhan Mantri Jan Arogya Yojana (PM-JAY). The implementation of PM-JAY resides with the National Health Authority (NHA). However, the use of the PM-JAY platform to its full potential is contingent upon the availability of robust evidence which can be used to set priorities and allocate resources to obtain the best value for limited available resources.
Recognizing the need for good quality cost data in setting reimbursement rates for services covered by PM-JAY and as an essential ingredient for conducting Health Technology Assessment (HTA) in the country, the government invested in the production of cost data and supported the concurrent development of a national database of healthcare costs: the National Health System Cost Database (NHSCD).
In this blog, we briefly describe India’s cost repository and how it caters to the needs of policymakers and researchers. We share examples of health system applications of the cost database and their policy implications, demonstrating the value brought about by this initiative. Finally, we conclude by highlighting the key areas that need to be addressed in order to improve the quality and sustain the relevance of the information the database offers, and promote the use of such initiatives for evidence-informed decision-making.
What does India’s healthcare cost repository offer?
A cost database is a public good to inform evidence-based decisions and economic evaluation research by providing access to a transparent set of country-specific reference costs. India’s cost repository is being established to offer access to national cost data on primary care provisioning through community health centres, primary health care and sub-health centres, and hospital-based secondary and tertiary care from both public and private providers. The development of NHSCD, a collaborative effort by the Postgraduate Institute of Medical Education and Research, Chandigarh, India; the Department of Health Research, India; and the Centre for Global Development, has facilitated the process of collating all these data into a single dataset and promoting their use and application. This initiative will make the average health facility cost data collected from multiple states freely available for researchers and policymakers.
The National Health System Cost Database
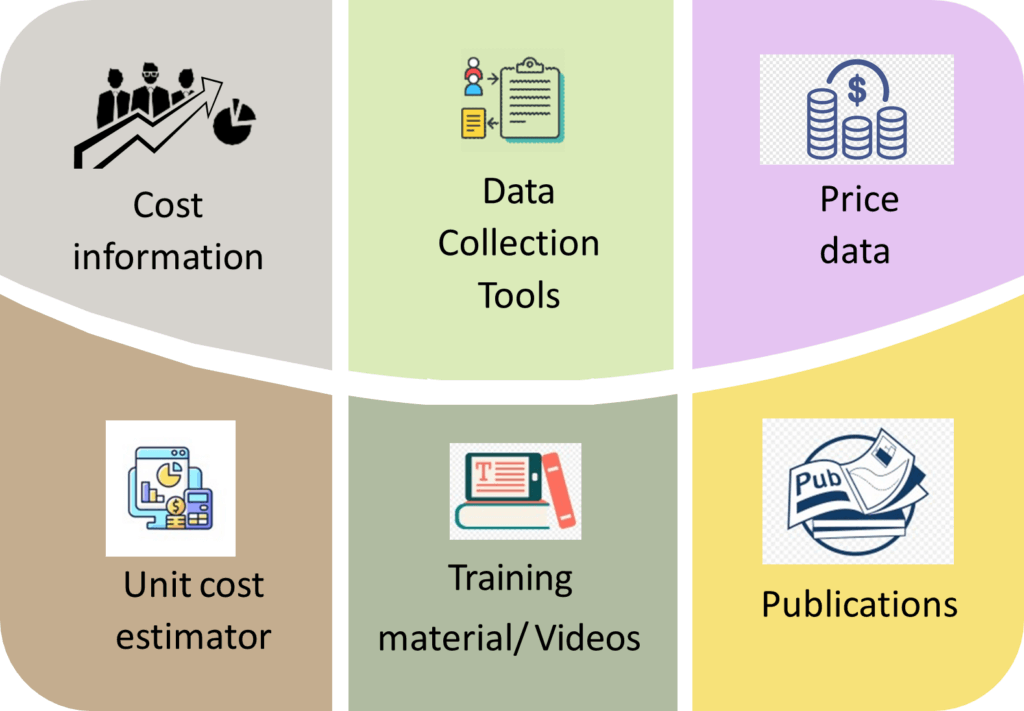
The cost data within this database provides annual and average healthcare facility costs at different levels of healthcare delivery (i.e., the value of all input resources used to produce a service), input-wise as well as broken down by different services. Another feature available on this web-based platform is the “unit cost estimator” which based on a set of key variables known to influence the unit cost, generates an average or unit cost in the form of cost per outpatient visit or inpatient admission for different states in India. The platform also hosts a costing manual and training videos on cost analysis. The data collection tools and the methodology deployed to estimate these costs have also been made available on the website to ensure transparency and for use and application by other practitioners. Moreover, the website also provides links to useful publications and resources in the context of costing and economic evaluations.
The utility of cost data systems for healthcare: applications and implications
The cost repository and the data held have been used in a number of ways that demonstrate its value (Figure 2). Cost data are valuable inputs to the conduct of HTA as well as budget impact assessment. More importantly, such data also aid the setting of reimbursement rates for various healthcare services. Three examples are described below.

- What is the optimal reimbursement rate for healthcare services?
As India established PM-JAY, a system for calculating reimbursement rates that adequately reflected the cost-of-service provision was needed. In view of this, HTAIn (the HTA Unit of the Government of India) at the Department of Health Research commissioned the Costing of Health Services in India (CHSI) study to estimate the costs of PM-JAY health benefits packages. The cost evidence generated from this study was used in revising the initial set of reimbursement prices. The CHSI study data were used to analyse the difference between existing reimbursement prices and costs so that the two could be aligned. Also, the data were used to identify variance in cost based on types of providers and their geographical locations, and inform a price weight scheme that compensates providers according to these factors.
- The cost implications of strengthening primary health care
Another pivotal component of the Ayushman Bharat scheme has been the setting up of Health and Wellness Centres (HWCs) for strengthening primary care in the country, the operationalization of which has been planned in a phased manner. For the scaling up of HWCs, it is fundamental to understand the resource requirements to assess the budgetary implication for the government. The cost data from the costing repository have been used to estimate the financial implications of this strategy over the next five years.
- Making HTA evidence more robust
The data from the cost repository has facilitated the growth of HTA in India by providing healthcare unit costs. For example, this data was used in the assessment of the cost-effectiveness of the typhoid conjugate vaccine (TCV) in children over six months of age, and a cost-effectiveness analysis of population-based screening for diabetes and hypertension in India. Both these studies demonstrate wider level policy implications of costing and HTA, where the former was conducted to aid policy-level decisions undertaken by India’s National Technical Advisory Group on Immunisation (NTAGI) as well as the Ministry of Health at the Central and State levels, and the latter was aligned with the government’s aims to expand primary care for diabetes and hypertension through the HWCs.
The challenges ahead
While a central repository reduces the transaction costs of obtaining cost information for a range of activities in healthcare decision making, the data embedded within the NHSCD must be expanded and updated regularly given continuous healthcare reforms as well as rising healthcare costs. Further, to model costs, it is pivotal to understand what is meant by costs and how it differs from prices. More importantly, the level of granularity of availability of records due to lack of electronic patient records extends the effort to determine costs by many folds, which is a deterrent to good quality cost data. Therefore, the government of India needs to focus on building sustainable mechanisms for setting up systems for generating accurate cost data rather than relying on resource intensive studies for cost data collection.
Secondly, to promote the use of standardized cost evidence as inputs for HTA, an issue of paramount importance is that the existence of the cost repository reaches, is accepted, and used by the research community and policymakers. Finally, it is worth acknowledging that there still exists an aperture between the researchers and policymakers, especially in terms of understanding cost evidence. Hence, it is all the more important that the existing and forthcoming data systems ensure relevance, validity, smooth usability, and practicability.
Conclusion
As the Indian health system embarked upon adopting an evidence-informed and inclusive health policy, it identified the lack of cost evidence as one of the key gaps requiring attention. The development of the cost repository is one of the crucial steps in providing access to transparent, country-specific reference costs, and has proved to be an invaluable resource for priority-setting and decision-making.